
Ipilimumab
Các tên gọi khác (4
) :
- MDX-010
- MDX-101
- MDX-CTLA-4
- MOAB-CTLA-4
Thuốc điều trị ung thư
Thuốc Gốc
Biotech
CAS: 477202-00-9
ATC: L01XC11
CTHH: C6572H10126N1734O2080S40
PTK: 148 kDa
Nhận Dạng Quốc Tế & Đặc Tính Hóa Học
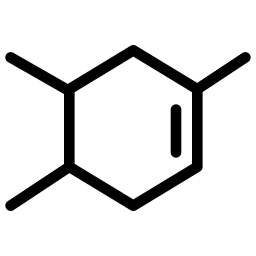
Công thức hóa học
C6572H10126N1734O2080S40
Phân tử khối
148 kDa
Dược Lực Học :
Cơ Chế Tác Dụng :
Dược Động Học :
In one pharmacokinetic study of patients with unresectable or metastatic melanoma peak concentrations, trough concentrations, and area under the curve (AUC) were found to be dose proportional in the dosage range examined (0.3, 3, or 10mg/kg every 3 weeks for four doses).
▧ Volume of Distribution :
Volume of distribution at steady state = 7.21 L
▧ Metabolism :
The metabolism of ipilimumab does not involve the cytochrome P450 enzyme system. Because ipilimumab is a protein it is expected to be degraded into small peptides and amino acids by proteolytic enzymes.
▧ Half Life :
Terminal Elimination Half-life: 14.7 -15.4 days
▧ Clearance :
Clearance was measured to be 15.3mL/hr-16.8 mL/hr. In one pharmacokinetic study examining ipilimumab administered every 3 weeks, clearance was found to be time invariant. Minimal systemic accumulation was observed (accumulation index of 1.5 fold or less). Steady state concentrations was reached by the third dose. Clearance will increase with increasing body weight; however, no dose adjustment is needed if administration occurs on a mg/kg basis. The following had no clinically meaningful influence on clearance: Age (range 26-86 years), gender, creatinine clearance (if ≥29ml/min), baseline AST, total bilirubin, ALT levels, concomitant use of budesonide, performance status, HLA-A2*0201 status, positive anti-ipilimumab antibody status, prior use of systemic anticancer therapy, baseline lactate dehydrogenase levels.
Độc Tính :
Chỉ Định :
Tương Tác Thuốc :
- Vemurafenib Consider therapy modification due to enhanced hepatotoxicity of vemurafenib
Liều Lượng & Cách Dùng :
Injection - Intravenous - 50 mg/10 mL, 200 mg/40 mL
Dữ Kiện Thương Mại
Nhà Sản Xuất
-
Công ty : Bristol-Myers SquibbSản phẩm biệt dược : Yervoy
Tài Liệu Tham Khảo Thêm
drugbank
National Drug Code Directory
Wikipedia
Drugs.com
Bạn thấy hài lòng ?
Bạn chưa hài lòng ?
... loading
... loading